4/24/2023
|
From a doctor’s point of view
It’s been a year since our practice was acquired by a PE-backed MSO.
[NK note: MSO = Managed Services Organization and handles a lot of the back office tasks for practices]
I can honestly say nothing has changed for me clinically. I still practice the same as I did before the acquisition, and there is no PE overlord in a business suit (or zip up vest) standing over my shoulder. There have been some changes to consolidate the back end part of the operations across the platform which honestly has been a breath of fresh air. The reality is that many practices are just not efficiently and well run from a business perspective – even large Orthopedic practices. As you state in the article, the MSO is very concerned with compliance and doing things above board, especially when it comes to billing, coding, and other requirements. They understand the level of scrutiny and do not want to risk anything that would stand in the way of a future sale or be a red flag to a buyer or regulator.
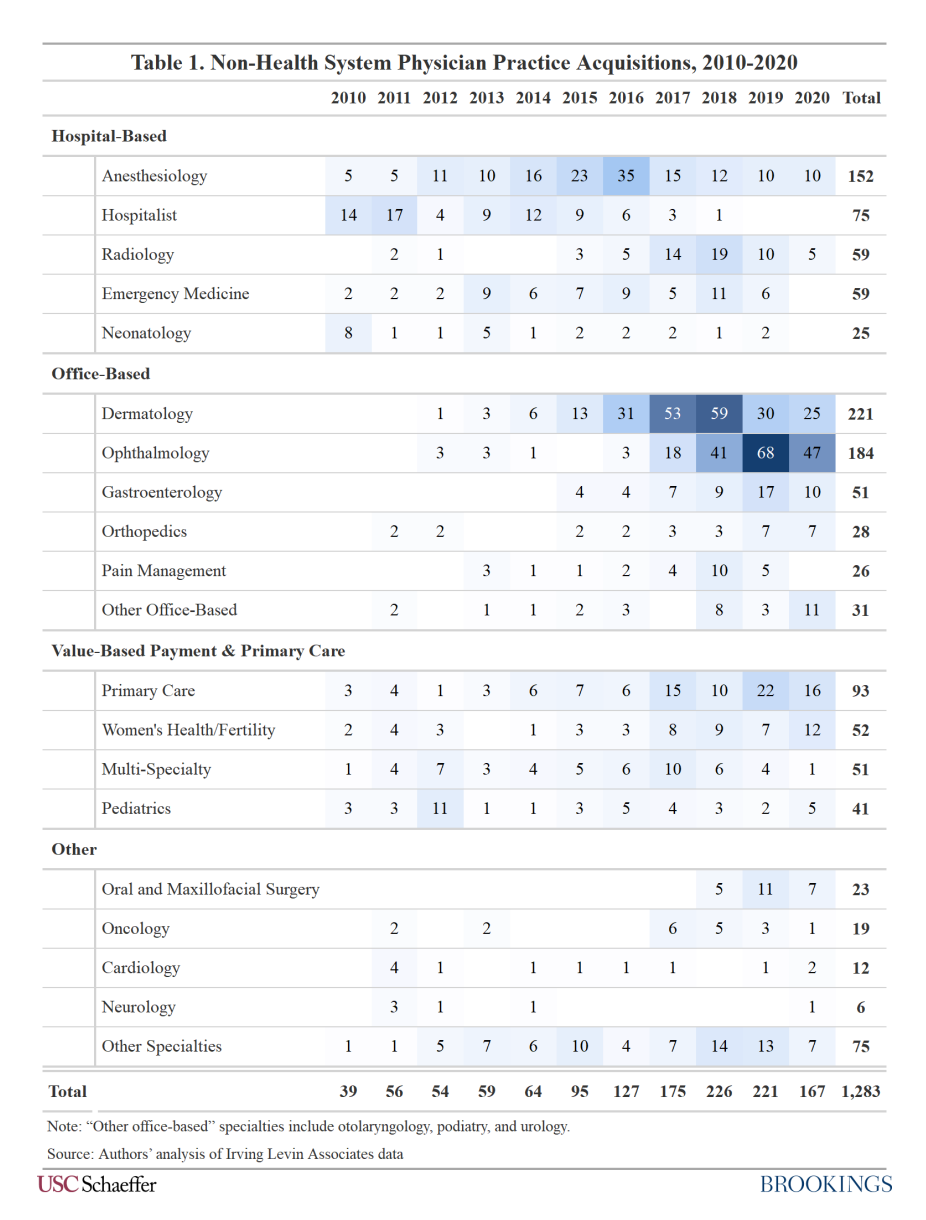
PE interest in Ortho is, I suspect, going to continue to grow. The commonly cited reasons include an aging (and increasingly obese) population, ability to leverage ancillary services, and relative fragmentation of the market. The real answer is that PE sees the huge opportunity in surgical case migration to the ASC [ambulatory surgery center] setting, especially lucrative joint replacement and spine procedures. In theory, this could be a win-win for docs, the MSO platform, patients, self-insured employers, commercial payors, and CMS. As you know, migrating the cases to an owned ASC means capturing the sweet, sweet facility fee (on top of the professional fee). ASCs are less expensive than big hospitals and health systems for these cases (on the order of tens of thousands of $).
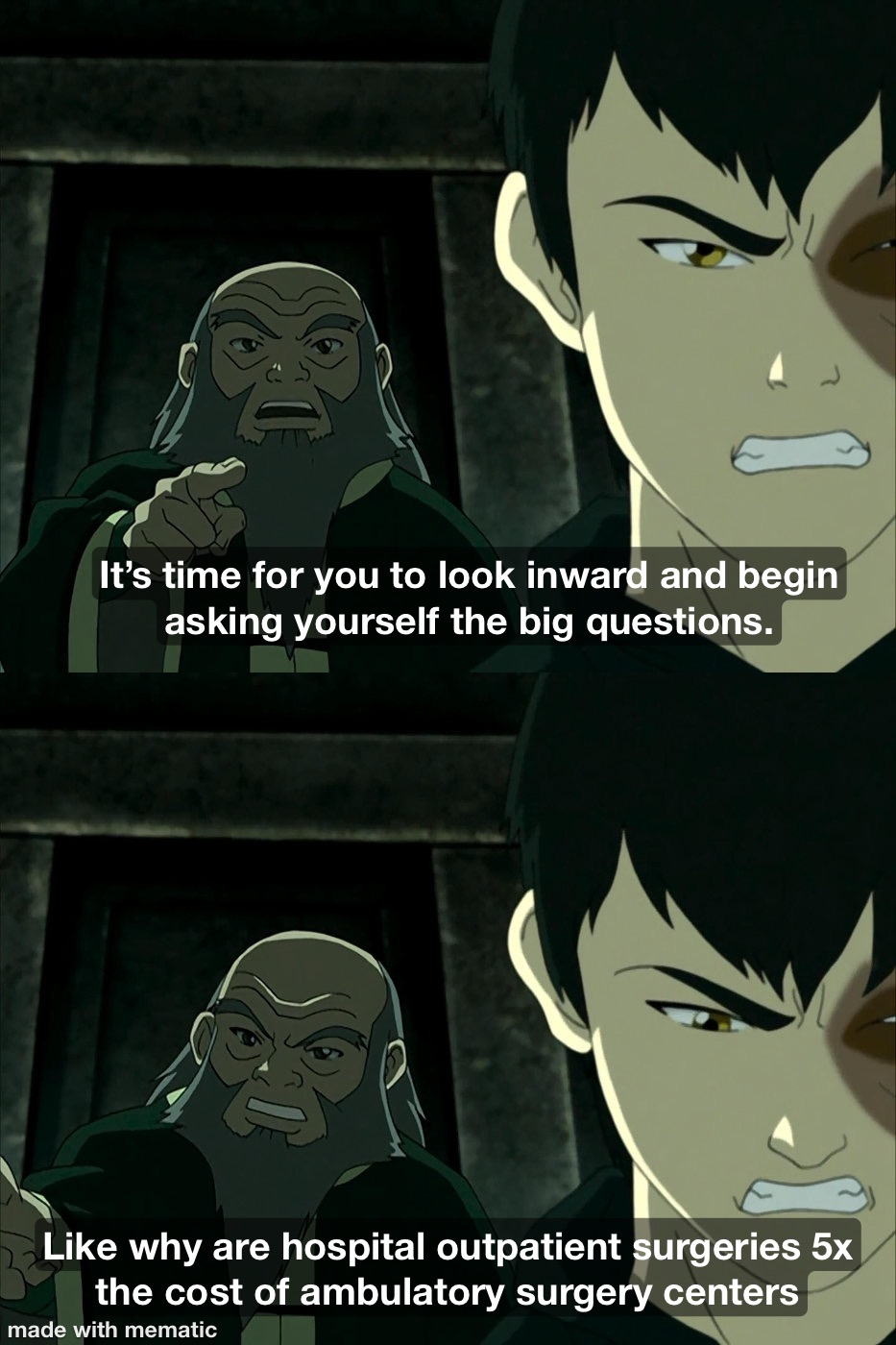 |
If a PE-backed MSO platform can help surgeons drive more volume (safely and clinically appropriate, of course) to the ASC, the platform can grow revenue, the inscos/employers save money, and patients get what often is a safer and better experience. The loser is the hospital/health system. MSO platforms can leverage economies of scale to reduce Ortho implant costs and supply costs, negotiate platform-wide pricing/reimbursement, and set up value-based arrangements (again, in theory improving reimbursement and reducing costs if you can do a good job).
(An interesting side point – we have tried to engage commercial payors for VBC, and it’s a lot harder than people think. I think it’s fair to ask at this point if commercial payors really want VBC or if they simply want to shift risk onto providers. The programs they offer come with upside/downside risk that is so unfavorable it doesn’t make sense to leave FFS.)
Whether or not PE-backed MSOs are going to achieve the goal of reducing costs in Ortho by siphoning business from health systems remains to be seen. But they can achieve revenue and EBITDA growth in MSK (this is the ultimate goal after all) without having to resort to some of the shenanigans we’ve seen in other specialties like Derm and ER.
For me, the biggest question is what happens after the 2nd, 3rd, or 4th sale of the platform. At some point, achieving ROI becomes increasingly difficult once you’ve maximized revenue without resorting to shady tactics. That’s when you get cost-cutting, corner-cutting, punishing OON contracts, over-imaging, overuse of procedures, etc.
-Anonymous
[NK note: I feel physically sick because I can read all of the acronyms above and not flinch. I need to go outside and touch grass.
I think orthopedics is somewhat unique because the surgeons have outsized sway with hospitals and for referrals. Plus the cost difference between getting a surgery done in a hospital vs. non-hospital setting is massive. But maybe this shows a playbook in one specialty where PE can help clinicians with independence. Over time we might see this expand further to other specialties (e.g. risk-bearing primary care).
Though I’m also curious how the PE-backed MSO generally plans to recoup its investment – if it’s just selling to a larger PE firm eventually then what happens?]
Is PE-owned independent or not? A question of governance
“ This is a compelling topic. A few thoughts:
- An issue I have with structural analyses like this generally: PE (like hospitals/systems and even health insurers) is not monolithic. Different PE groups have different goals and philosophies and are run by variably competent teams. That makes it extra hard to generalize at the category level.
- I think in general, healthcare is having a long-term existential crisis with the profit motive vs the mission motive. PE, like for-profit hospitals, is a natural magnet for those kinds of concerns.
- The “corporatization” and scaling up of healthcare organizations issue is distinct from profit issues. Not for profit health systems have this as a cultural/operational pain point and have for years. And the small, medium, and large independent physician groups being acquired by PE are not suddenly going for-profit; they were all already for-profit entities; people forget this. The difference between a for-profit independent medical group and one that is owned or part-owned by PE is “well it depends”, but on balance probably the big difference is governance (no longer solely self governed) capital, scale and systematization. Plus the shorter time horizon for profits.
- PE is also putting stress on a historically meaningful concept of “independent” practice. I was once in a meeting of an industry group comprised of independent medical groups of a certain specialty. They were internally debating whether some of their long-time colleague practices needed to be ejected from membership in the group if they became part-owned by PE. No conclusion was reached.”
-Amanda Berra, EVP Union Healthcare Insight
[NK note: The crux of most responses I got was “how do I unsubscribe”. But the second most popular was “healthcare doesn’t know if it’s a for-profit or mission oriented industry”. That’s what causes the dissonance – the entrance of PE who very much views this as for profit while others view it as mission driven.
Also what if you consider your mission to be making money? I’ll let you take a second to sit with that one and digest.
I think the question of governance is a good one too. In many cases PE really wants the doctor to continue doing their thing and needs the doctor to be happy. In other cases, there seems to be more heavy-handedness (anecdotally).]
 |
Private equity’s use of a self-enriching capital structure
“I like the objective consideration of how PE vs. health systems attempt to increase value in healthcare companies (e.g., referrals, staffing, etc.) and agree that it makes sense to evaluate case by case. I don’t think PE is unique in trying to maximize profits in healthcare, and I don’t think profit maximization is necessarily value destructive (like your CareMore example). But what I didn’t see in the post — and what I think is particularly problematic about PE — is that PE often destroys value in acquired companies by irresponsibly playing around with their capital structure. And playing with capital structure is, after all, the basic premise of PE.
A great example in healthcare is Weight Watchers: it was purchased in an LBO in 1999 and the buyers not only levered up the company as part of that transaction but then also added massive amounts of debt in the early 2000s to give the owners liquidity through share buybacks. Now that interest rates have risen and WW’s core business is in decline, WW has an unmanageable debt load and real solvency concerns. So while PE management may have been acting in (PE) shareholders’ best interest with the buybacks, they mismanaged the company’s fundamentals, and therefore long-term shareholder value, by taking on so much debt. A similar (non-healthcare) example is the story of how Jay Powell acquired a manufacturing company called Rexnord when he was at Carlyle and massively destroyed value by loading up Rexnord with unsustainable amounts of debt. Carlyle still managed to sell the company for a $900M profit — this Fortune article has a good summary of the story.
So overall I don’t think the problem with private equity is that it tries to make companies more efficient or that it tries to increase profits. I think the problem with private equity is private equity — the mechanics of the leveraged buyout model and how the incentives of PE buyers and their acquired companies can diverge in destructive ways.”
[NK note: I guess WW was really lugging around some “debt weight” huh. Or a joke about shedding a few billion. Idk.
I sort of alluded to the 3-5 year time horizon issue in my post, but I think this makes more explicit what the downside is here with good examples. If you can use a tool to enrich yourself in 3-5 years while destroying the long-term value of a company long after PE sells, then that is bad.
It seems like one of the core issues with this is that there really isn’t an incentive to invest in R&D if you’re just trying to generate as much cash as possible in a 3-5 year timeline. And by choosing debt, which has a regular amount you need to pay back in the form of interest, it becomes hard to invest in things with unclear payback timelines like R&D.]
Hospitals should learn from PE-owned groups to be competitive
“Nikhil, I appreciated this rare, nuanced take on PE’s impact within healthcare. This is something we are watching play out in real time at Zocdoc.
In looking at our data, which is a reflection of what is happening in the market, there is a significant and rapid mix shift between large provider groups (LPGs) and hospitals and health systems (HS). In 2019, the share of bookings in our Enterprise segment — composed of LPGs and HS, as opposed to smaller independent practices — was split ~50/50 between the two groups. Year to date in 2023, that mix has shifted to ~80/20 LPG. Given that ~85% of Zocdoc bookings last year were made with a commercial insurance plan, LPGs are disproportionately reaping these benefits.
[NK note: The large practice groups have a much higher PE ownership]
I have every reason to believe this trend will continue to the detriment of HS who have “no mission without a margin.” My take is that to remain competitive, there is a lot that hospitals and health systems should learn quickly from these PE-backed large provider groups: they are rational economic actors, they find and replicate successful playbooks, and they are clear-eyed and quick decision-makers. To give you a sense of the speed difference, LPGs make the decision to join Zocdoc 5x faster than HS.”
-Oliver Kharraz, CEO of Zocdoc
[NK note: It seems like PE firms are now shifting from captive audience areas where the patient doesn’t have a choice (e.g. anesthesia and surprise bills) to areas where there is more “consumer choice” (e.g. derm, ophthalmology, primary care). I’d guess part of this strategy is to make it easier to get patients in through the door. Wait were private equity firms really the harbingers of “healthcare consumerism” the whole time?]
What is the end game for private equity?
“I left PE for a bunch of reasons, but part is that healthcare services PE (which is what I think you’re focused on, there’s a lot of other really different healthcare PE this applies less to) really didn’t have many levers for value creation that I thought additive to society at large. Like the selling point for a lot of healthcare PE professionals is often “hey I like PE but want to work in a sector where it has some meaning” and then the game is “multiple arbitrage through mindlessly slapping together provider groups in a given sector and hoping to sell at a better multiple than you bought”.
Literally, at Wharton a VP at PE group leading a derm clinic rollup presented right when we entered and half of the HCM class was like “wow, this is fundamentally dissociated from why I like healthcare, you do nothing to change or better this space” (many HCMers enter Wharton as idealists, ha).
Literally any healthcare PE guy or gal who tells you they add value other ways is 95% chance of being full of it. Doctors have max capacity, the amount of value added through systems and “professionalization” is limited, and adding new service lines leads to the phenomena you describe of overprescribing, etc. (worth noting that we killed a few derm acquisitions because we didn’t like their Mohs referral trends, but we might’ve been exception to the norm, at least then).
Here’s the biggest thing – I don’t see an endgame here. Eventually doctors get out of employment agreements and there’s burnoff. Scale doesn’t really have much advantage unless you can bang the insurers back, which IDK that any of these groups do even at highest level. There’s no logical acquirers in most cases. And we’ve seen how these kind of rollups do on public markets previously. I don’t know how it resolves, but feels like a few not great blowups”
-Anonymous
[NK note: Let’s be honest, we know the end game…]
 |
Thinkboi out,
Nikhil aka. “I miss when PE meant gym class to me”
Twitter: @nikillinit
Other posts: outofpocket.health/posts